Preimplantation Genetic Diagnosis (PGD) represents a groundbreaking advancement within the landscape of in vitro fertilization (IVF), offering a sophisticated method to assess the genetic health of embryos before implantation. This innovative technique has revolutionized assisted reproductive technologies by allowing prospective parents to make informed decisions regarding the selection of embryos free from specific genetic abnormalities or disorders. PGD goes beyond traditional prenatal testing, providing a comprehensive understanding of an embryo’s genetic makeup at an early stage.
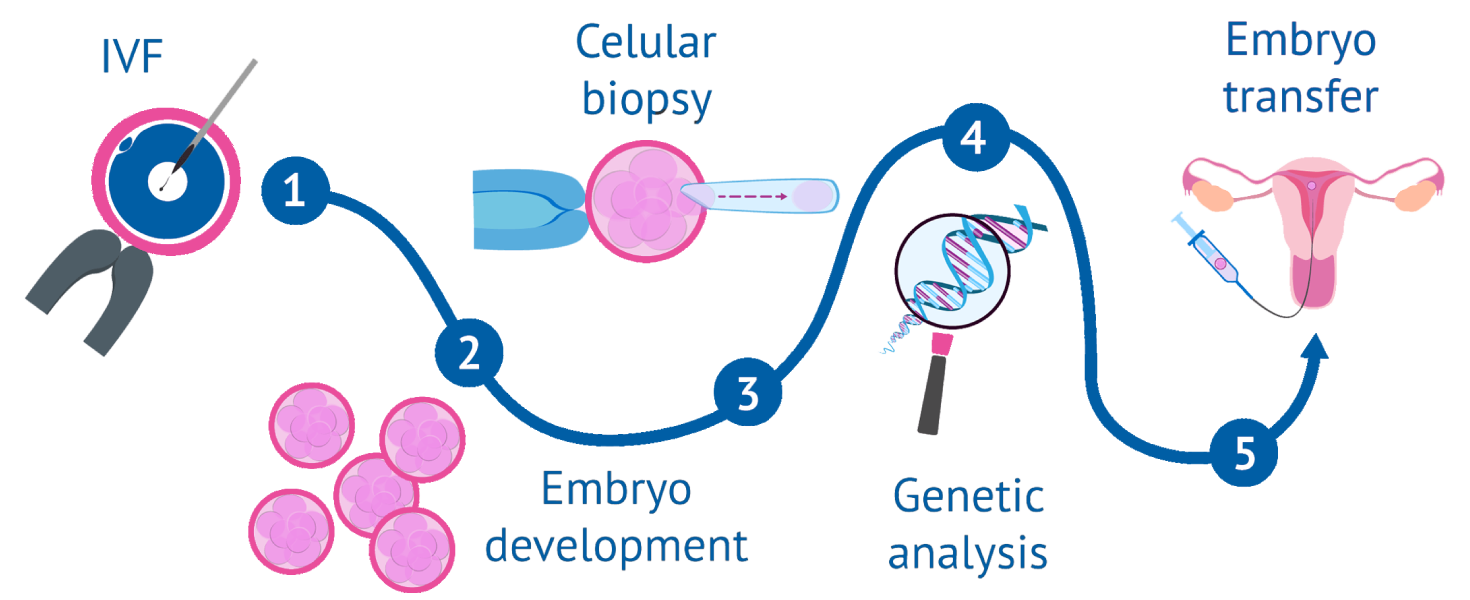
The process of Preimplantation Genetic Diagnosis (PGD) involves a series of intricate steps to analyze the genetic composition of embryos created through in vitro fertilization (IVF).
Before beginning the PGD process, individuals or couples undergo genetic counseling to understand the specific genetic condition, its inheritance pattern, and the implications for their offspring.
The process starts with ovarian stimulation using fertility medications to induce the development of multiple eggs. Once the eggs are deemed mature, a minor surgical procedure is performed to retrieve the eggs from the ovaries.
The retrieved eggs are then fertilized with sperm in the laboratory, and the resulting embryos are cultured for several days, typically to the blastocyst stage.
At the blastocyst stage, a few cells are carefully removed from the trophectoderm (the outer layer of the embryo) through a biopsy procedure. This biopsy does not harm the inner cell mass, which will develop into the fetus.
The cells obtained from the biopsy are processed to extract genetic material, usually DNA, which carries information about the genetic composition of the embryo.
The extracted genetic material undergoes advanced genetic analysis techniques, such as polymerase chain reaction (PCR) or fluorescence in situ hybridization (FISH). This analysis aims to identify the presence or absence of the specific genetic condition being targeted.
Based on the genetic analysis, embryos are classified into different categories, such as unaffected, carrier, or affected by the specific genetic condition. Only embryos free from the targeted genetic condition are considered for transfer.
The primary goal of PGD is to select embryos that are free from specific genetic abnormalities or disorders. These genetically normal embryos are considered more likely to result in a healthy pregnancy.
In cases where additional viable embryos are obtained, they can be cryopreserved for future use, reducing the need for additional ovarian stimulation and egg retrieval in subsequent IVF cycles.
The selected genetically normal embryos are then transferred into the uterus of the intended mother or a gestational carrier to establish a pregnancy.
In conclusion, Preimplantation Genetic Diagnosis (PGD) emerges as a game-changing pillar in the landscape of assisted reproductive technologies, providing individuals and couples with the power to shape their family’s genetic destiny. Beyond its technological prowess, PGD stands as a beacon of hope, offering a meticulous approach to family planning by enabling the selection of embryos free from specific genetic disorders. The detailed insights gained through PGD not only minimize the risk of passing on hereditary conditions but also foster informed decision-making and a sense of control over one’s reproductive journey. As a tool that aligns with ethical considerations, PGD embodies the fusion of scientific advancements and compassionate family-building, reshaping the narrative of reproductive possibilities. Through the lens of PGD, the future of family planning is not only about overcoming biological challenges but also about embracing a future where healthier generations can thrive.
